Discover how Ozempic supports sustainable weight loss by curbing appetite, improving metabolism, and delivering real, lasting results.
If you’ve been on a weight loss journey and feel like nothing is working, you’re not alone. The market is flooded with fad diets, miracle supplements, and fitness programs that promise results but rarely deliver sustainable success. But what if there was a prescription medication that could actually help you lose weight and keep it off? Enter Ozempic—a groundbreaking treatment initially developed for type 2 diabetes that’s now taking the weight loss world by storm. In this deep dive, we’re unpacking everything you need to know about Ozempic: what it is, how it works, and why it might just be your key to lasting weight loss.
Understanding Ozempic: What Is It?
The Origin and Purpose of Ozempic
Ozempic, generically known as semaglutide, was originally created to manage blood sugar levels in adults with type 2 diabetes. Developed by Novo Nordisk, this once-weekly injectable medication has quickly gained attention for an unexpected benefit: significant and sustained weight loss in many users. Though its primary intention was glycemic control, clinical observations revealed that patients were consistently losing weight as a side effect—prompting deeper research into its weight-reducing potential.
Semaglutide mimics a naturally occurring hormone in the body called GLP-1 (glucagon-like peptide-1), which is released in the gut and influences insulin production, appetite, and food intake. This mimicry not only helps in regulating blood sugar but also in reducing hunger and increasing feelings of fullness.
Over the last few years, Ozempic has evolved from a diabetes treatment into a hot topic in the world of medical weight loss. It’s often compared with its sibling medication Wegovy, which contains the same active ingredient but is specifically approved for weight loss.
Active Ingredient and How It Works
Semaglutide is the powerhouse behind Ozempic. As a GLP-1 receptor agonist, it interacts with the body’s natural systems to lower blood sugar levels by boosting insulin secretion and reducing the amount of glucose produced by the liver. But what really stands out is how it affects appetite regulation.
Once injected, semaglutide acts on receptors in the brain that control hunger. Users often report a significant drop in cravings, a lower desire to eat large meals, and even aversions to certain high-calorie foods. The slow and steady nature of how semaglutide works helps people eat less naturally, without forcing themselves through starvation diets or intense calorie counting.
Moreover, semaglutide slows down gastric emptying, meaning food stays in your stomach longer. This adds to the feeling of fullness and helps reduce snacking or second helpings. It’s not a magic pill, but it definitely makes the weight loss process a lot more manageable.
FDA Approval and Medical Uses
Ozempic was approved by the FDA in December 2017 for the treatment of type 2 diabetes. Since then, it’s been widely prescribed not only for managing blood sugar but also for reducing the risk of major cardiovascular events like heart attacks and strokes in people with type 2 diabetes and established heart disease.
While not officially labeled as a weight loss drug under the Ozempic brand, doctors have been prescribing it off-label for obesity treatment. That’s because of the growing evidence—and patient results—that prove its effectiveness in promoting weight reduction. The weight-loss-specific brand Wegovy was later approved by the FDA in 2021, solidifying semaglutide’s reputation as a powerful tool in obesity management.
In short, Ozempic started as a diabetes medication but quickly became a dual-purpose drug, offering both metabolic control and substantial weight loss potential.
Ozempic as a Weight Loss Aid
How Ozempic Supports Weight Loss
Ozempic helps users lose weight by controlling two things: blood sugar levels and appetite. But let’s break that down a bit. First, by improving insulin sensitivity and lowering blood glucose, the body becomes more metabolically efficient. Second—and more crucially for weight loss—it reduces hunger signals sent from the brain.
Have you ever tried to diet and felt like you were constantly thinking about food? That’s where Ozempic changes the game. The medication works on the hunger centers in your brain, making food less tempting and overindulgence less likely. Instead of battling willpower every hour, users often describe feeling satisfied with much smaller portions and fewer meals.
Also worth noting, Ozempic’s impact is cumulative. This isn’t about rapid, unsustainable weight loss. Over weeks and months, the consistent effects on appetite and metabolism lead to gradual, long-term changes in body composition.
Many users report weight loss ranging from 10% to 15% of their total body weight over several months. For someone who weighs 200 pounds, that could mean losing 20 to 30 pounds in a sustainable, manageable way—without resorting to crash diets or extreme exercise regimens.
Difference Between Ozempic for Diabetes and Weight Loss
While Ozempic and Wegovy both contain semaglutide, the key difference lies in their dosage and intended use. Ozempic typically maxes out at a weekly dose of 2 mg for diabetes treatment, while Wegovy can go up to 2.4 mg for weight loss.
Doctors often prescribe Ozempic off-label for weight management because of its proven track record. The lower dose still works for many individuals, especially when combined with lifestyle changes like diet and exercise. However, for those needing a more aggressive weight loss approach, Wegovy might be the preferred option due to its higher dosing range.
That said, not everyone qualifies for Wegovy, and insurance coverage varies. This is why many people begin their weight loss journey with Ozempic under the supervision of a healthcare provider. The goal is to find a dosage that supports weight loss while minimizing side effects.
Clinical Trials and Success Stories
Numerous clinical trials have confirmed Ozempic’s effectiveness for weight loss, even among people without diabetes. In one study, individuals taking semaglutide lost an average of 15% of their body weight over 68 weeks. Compare that to the placebo group, which only lost around 2.4%, and the results speak for themselves.
But beyond the data, real-world stories add a human touch. People who struggled for years with weight gain, emotional eating, or failed diets have finally found success using Ozempic. Some describe it as the “missing piece” in their health journey—a tool that gave them control without the usual mental and emotional exhaustion of dieting.
These stories are echoed across social media platforms and medical forums, with users sharing photos, updates, and tips. While results vary by individual, the consensus is clear: Ozempic works when used consistently and responsibly.
The Science Behind Ozempic
GLP-1 Receptor Agonists: What They Do
To really grasp why Ozempic works so well, you need to understand the science behind GLP-1 receptor agonists. GLP-1 stands for glucagon-like peptide-1, a hormone your body naturally produces after eating. This hormone has several roles, but its biggest claim to fame is that it helps regulate blood sugar and reduce appetite. That’s exactly what semaglutide—the active ingredient in Ozempic—is designed to mimic.
Once semaglutide enters your bloodstream, it binds to GLP-1 receptors in various organs, including the pancreas, brain, and stomach. In the pancreas, it promotes the release of insulin and suppresses the release of glucagon, which keeps your blood sugar levels stable. In the brain, it triggers the “full” signals that tell you to stop eating. And in the stomach, it slows down digestion, so food stays longer in your system, making you feel full for extended periods.
This multi-pronged approach makes GLP-1 receptor agonists like Ozempic highly effective for both blood sugar control and appetite suppression. It’s like hitting three birds with one stone—managing diabetes, reducing cravings, and promoting satiety.
Impact on Appetite and Satiety
One of Ozempic’s standout effects is its impact on appetite control. For most people trying to lose weight, constant hunger and cravings are the biggest roadblocks. Dieting often leads to a cycle of restriction, binging, and guilt—something Ozempic helps to break.
The drug communicates with the hypothalamus, the part of the brain responsible for hunger and energy balance. It tells your brain that you’re full, even if you’ve eaten less than usual. That means smaller portions feel satisfying, and mindless snacking becomes less tempting.
In clinical settings, patients often say they simply “don’t think about food as much” when on Ozempic. This is a major shift from the usual diet mentality, where you’re counting calories, obsessing over meal plans, or feeling deprived. Instead of fighting your body, Ozempic helps align your biology with your weight loss goals.
Not only does it reduce physical hunger, but it may also help curb emotional or stress-related eating. The result? More control over what, when, and how much you eat—without the mental tug-of-war.
Effects on Blood Sugar and Insulin
While Ozempic is primarily prescribed for type 2 diabetes, even non-diabetic users benefit from its blood sugar-lowering effects. Stable blood sugar means fewer spikes and crashes, which are often responsible for sudden hunger, energy dips, and sugar cravings.
When you eat, your body breaks down carbohydrates into glucose, which enters the bloodstream. Normally, your pancreas responds by releasing insulin to help move that glucose into cells for energy. But if you’re insulin resistant or have erratic blood sugar levels, this process goes haywire. That’s where Ozempic comes in.
Ozempic enhances insulin sensitivity and ensures your body responds appropriately to food intake. It helps your liver produce less glucose and promotes more efficient energy usage. For weight loss, this means fewer cravings for high-carb or sugary foods and more steady energy throughout the day.
Over time, better blood sugar control can improve your metabolic health, reduce inflammation, and support long-term fat loss. So, even if you’re not diabetic, these physiological improvements play a huge role in sustainable weight management.
Starting Your Ozempic Journey
Who Should Consider Ozempic?
Ozempic isn’t for everyone, but it can be a game-changer for many. If you’re overweight or obese and have struggled with traditional methods of weight loss, Ozempic might be worth discussing with your doctor. It’s particularly effective for individuals who experience intense hunger, frequent food cravings, or insulin resistance.
The ideal candidates include:
Adults with a BMI over 30 (obese), or over 27 with a weight-related health condition like hypertension or sleep apnea.
People who haven’t seen lasting results from diet and exercise alone.
Those seeking a medically supervised alternative to bariatric surgery.
Type 2 diabetics who also want to manage their weight.
That said, there are important considerations. Ozempic is not suitable for individuals with a history of medullary thyroid carcinoma or pancreatitis. It’s also not recommended for pregnant or breastfeeding women.
The best way to determine if it’s right for you? Consult a healthcare provider who understands your medical history and can guide you through a personalized plan.
Getting a Prescription: What to Expect
The process of getting started with Ozempic usually begins with a consultation. You’ll likely speak with a general practitioner, endocrinologist, or weight loss specialist. During the appointment, expect to discuss:
Your current weight and BMI
Past dieting history
Medical conditions and medications
Lab work including A1C, liver enzymes, and kidney function
If the doctor deems you a good fit, they’ll prescribe a starting dose—usually 0.25 mg per week for the first month to allow your body to adjust. Over time, the dose may be increased gradually, depending on how you respond.
Once prescribed, Ozempic is available via pen injector—similar to an EpiPen—which you self-administer once a week in the abdomen, thigh, or upper arm. Most people find the injection process simple and virtually painless.
Insurance coverage can be tricky. Some plans may not cover Ozempic if it’s prescribed solely for weight loss. In such cases, Wegovy or a compounding pharmacy alternative might be explored.
Dosage and How It’s Administered
Ozempic comes in pre-filled pens with various dosages. Here’s how dosing typically progresses:
Week 1-4: 0.25 mg once a week (starter dose to reduce side effects)
Week 5 and beyond: Increase to 0.5 mg or 1 mg, depending on your goals and tolerance
Max dose: 2 mg weekly (for diabetes); higher doses under other brand names for weight loss
The injection is subcutaneous, meaning it’s delivered under the skin. You don’t need to go into a clinic—just pick a consistent day of the week, and inject at home. It’s best to rotate injection sites to avoid irritation.
One major advantage of Ozempic’s weekly dosing is convenience. You’re not popping pills daily or counting meal replacements—just one injection per week and you’re set.
Pro tips for smooth administration:
Inject at the same time and day each week.
Store the pen in the refrigerator, but let it come to room temperature before use.
Use alcohol wipes and follow instructions carefully.
Dispose of needles safely in a sharps container.
Realistic Expectations with Ozempic
Weight Loss Timelines
If you’re considering Ozempic for weight loss, you might be wondering: “How long until I see results?” The short answer? It varies. Some people notice a difference in appetite within the first week, while significant weight loss typically begins after 4–8 weeks. But like any sustainable change, this is a marathon—not a sprint.
The early weeks on Ozempic are often about adjustment. You’re starting at a low dose, your body is getting used to the medication, and your appetite is beginning to shift. Some users may drop a few pounds quickly due to reduced food intake, but the real magic happens over the long term.
Clinical trials show that most people begin to see measurable weight loss around the 2-month mark, with steady and consistent progress continuing through 6 to 12 months. On average, patients lose 10–15% of their body weight within a year. That’s significant, especially considering that even a 5–10% reduction can improve cholesterol, blood pressure, and energy levels.
The key is consistency. Missing doses or giving up too soon can derail progress. Ozempic isn’t a quick fix—it’s a tool that supports gradual, lasting change when combined with mindful eating and some physical activity.
So, what’s a realistic expectation? Aim for 1 to 2 pounds per week after the initial adjustment period. That might not sound dramatic, but it adds up fast—and unlike crash diets, it’s weight that’s more likely to stay off.
Understanding Plateaus
Plateaus happen—even with Ozempic. One day, the scale is moving steadily, and the next, it won’t budge for weeks. Frustrating? Absolutely. Normal? 100%.
Weight loss plateaus can occur for a variety of reasons: your metabolism may adapt to your lower calorie intake, your body composition is shifting (you may be gaining muscle while losing fat), or your lifestyle habits may need fine-tuning.
Ozempic can reduce appetite, but it won’t eliminate the need for movement and nutritional awareness. As your weight drops, your body requires fewer calories. If your intake and activity don’t adjust accordingly, progress can stall.
Here’s how to break through a plateau:
Track your food for a week to spot hidden calories.
Increase protein intake to support lean muscle.
Add variety to your workouts or increase intensity.
Evaluate stress and sleep, both of which impact hormones and metabolism.
Sometimes, plateaus are your body’s way of recalibrating. Give it time. Avoid drastic changes like cutting too many calories or overexercising. Stay on track with your Ozempic doses, and the scale will start moving again.
Most importantly—don’t let a plateau demotivate you. They’re a natural part of any weight loss journey. Celebrate the non-scale wins (more on that next), and keep your eye on the big picture.
Non-Scale Victories to Celebrate
Weight loss isn’t just about numbers. In fact, some of the most powerful wins don’t show up on the scale at all. These “non-scale victories” (NSVs) are signs that your body is changing in meaningful ways—and they’re often a better indicator of progress than a number.
Here are some common NSVs you might notice while using Ozempic:
Clothes fit better or you’re down a size.
Increased energy levels throughout the day.
Improved mobility—walking, climbing stairs, or exercising feels easier.
Better sleep and less snoring.
Lower blood pressure and improved cholesterol levels.
More confidence in social situations.
Fewer food cravings and better control over portions.
These changes often show up before significant weight loss does, especially in the early months of Ozempic use. They’re also incredibly motivating. When the scale isn’t cooperating, these wins remind you that your hard work is paying off.
Another tip: take progress photos and measurements. Sometimes your body is transforming in ways the scale can’t capture. Comparing side-by-side pictures over time can be a real confidence booster.
Focus on how you feel—stronger, more in control, and healthier. That’s the true measure of success.
Conclusion
Ozempic isn’t a miracle drug—but it is a game-changer. Whether you’re battling stubborn weight, chronic cravings, or the frustrations of failed diet after failed diet, Ozempic offers a scientifically-backed, sustainable path to real transformation. Its dual action on blood sugar and appetite makes it one of the most effective modern tools for weight loss.
But here’s the thing: Ozempic works best when you work with it. That means consistency with your weekly doses, making mindful food choices, and adding movement into your life. It’s not about perfection; it’s about persistence. The weight loss is gradual, the changes are real, and the benefits go far beyond the scale.
What sets Ozempic apart is that it doesn’t just force weight off—it teaches your body and mind a new way to interact with food and hunger. You’re no longer driven by cravings or ruled by your next meal. Instead, you regain control, and that power feels incredible.
If you’re thinking about starting Ozempic, talk to a healthcare provider. Make sure it’s the right fit for you, understand the commitment, and stay patient with your progress. The results won’t happen overnight, but with consistency, they will come—and they’ll stick.
Remember, this is your journey. Whether you’re down five pounds or fifty, every step forward matters. You deserve to feel good in your body, confident in your choices, and excited about your future. And Ozempic just might be the key that unlocks it all.
-
Hot-Sale
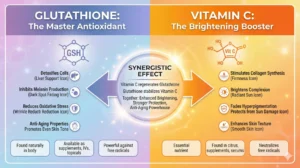
Asconex Vitamin C (Ascorbic Acid) IV/IM Drip for Antiaging, Melanin Suppression, Antioxidant and Skin Brightness Benefits
£38.00 – £70.00Price range: £38.00 through £70.00 Select options This product has multiple variants. The options may be chosen on the product page -
Hot-Sale
Glutanex Glutathione 1200mg IV Drip for Antiaging, Melanin Suppression, Antioxidant Skin Brightness Benefits
£65.00 – £120.00Price range: £65.00 through £120.00 Select options This product has multiple variants. The options may be chosen on the product page -
Hot-Sale
Glutanex IV Drip Set, Whitening Combination Kit with Glutathione, Vitamin C, Lipoic Acid for Antiaging, Skin Brightness Benefits
£30.00 – £250.00Price range: £30.00 through £250.00 Select options This product has multiple variants. The options may be chosen on the product page
FAQ
1. How quickly will I start losing weight on Ozempic?
Most people begin noticing a decrease in appetite within the first week, but significant weight loss typically starts between weeks 4 and 8, after your dose has been gradually increased. Expect a slow and steady pace—around 1-2 pounds per week is common once your body adjusts.
2. Do I need to follow a special diet while on Ozempic?
While there’s no specific “Ozempic diet,” healthier eating habits will definitely enhance your results. Aim for lean proteins, whole grains, fruits, veggies, and healthy fats. Try to limit processed foods and added sugars. Portion control becomes easier on Ozempic, but making smarter food choices will take your progress even further.
3. Are there any side effects I should be aware of?
Yes—common side effects include nausea, constipation, bloating, and sometimes fatigue. These often improve after the first few weeks or when the dosage is increased slowly. To minimize discomfort, eat smaller meals, stay hydrated, and avoid high-fat or greasy foods. Always consult your doctor if symptoms become severe.
4. Can I stop taking Ozempic once I reach my goal weight?
That depends. Some people transition off Ozempic and maintain their results through lifestyle changes, while others stay on a maintenance dose to prevent weight regain. It’s a conversation to have with your healthcare provider, based on your progress, habits, and long-term goals.
5. Is Ozempic safe for people without diabetes?
Yes. Although originally approved for type 2 diabetes, semaglutide (under the name Wegovy) is FDA-approved for chronic weight management in people without diabetes. Many doctors prescribe Ozempic off-label for this reason. Just make sure it’s done under medical supervision with regular check-ins.
Checkout our Facebook Page and leave your review about our Health Care Products.